
Date: 27 Jan 2026
When Joseph from Eldoret first heard his wife's cancer diagnosis, his first thought was, "What do I do now?" Not as a patient, but as a caregiver.
In Kenya, where family is everything, cancer becomes a family disease. The patient fights the illness, but the caregiver fights the battles the pharmacy runs, the hospital appointments, the 3 AM medication alarms, the silent worry of mounting costs.
Over 70% of cancer patients in Kenya rely on family members for daily care. Yet no one hands caregivers a manual.
You learn by doing, often while exhausted, scared, and overwhelmed.
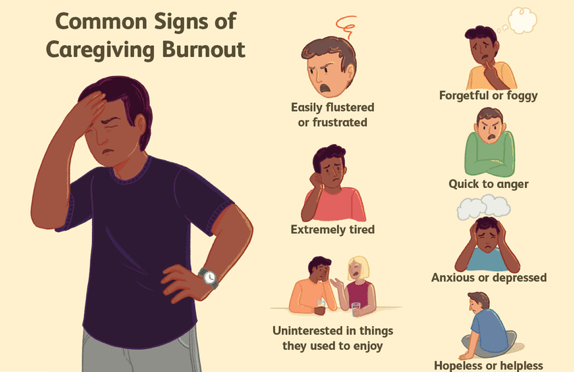
Caregiving is more than physical tasks. It's emotional labor that can leave you drained. Studies from Aga Khan University Hospital show that Kenyan cancer caregivers experience higher rates of depression and anxiety than patients themselves. You may feel:
Guilt for taking a break
Anger at the unfairness of it all
Grief for the life you had before
Isolation—friends don't understand
Financial strain that keeps you awake at night
Acknowledging these feelings is the first step. You cannot pour from an empty cup. Caring for yourself isn't selfish—it's necessary for sustainable care.
Designate one place (a notebook or phone app) for:
Medication schedule: Name, dose, time, special instructions
Doctor contacts: Oncologist, pharmacist, nurse, hospital lines
Symptom tracker: Note changes daily—pain levels, appetite, mood
Questions list: Add questions as they arise for next appointment
Financial log: Track expenses, insurance claims, receipts
This simple system prevents the chaos of scattered information when you need it most.
Cancer patients often take 5-15 different medications daily. Missed doses can derail treatment.
Set up a system:
Use a weekly pill organizer (available at Pharmily)
Set phone alarms with labels: "Pain medication—8 AM"
Keep a backup supply for critical drugs—never run out
Understand each drug's purpose and side effects
Pharmily's monthly refill service ensures you never run out. We track your prescriptions and deliver refills 3 days before you need them across Nairobi, Kisumu, Mombasa, and Nakuru.
Ask the hospital nurse to teach you:
How to take temperature and blood pressure correctly
When to call the doctor vs. manage at home
Proper wound care for surgical sites
How to give injections if needed (some pain medications)
Recognizing infection signs: fever over 38°C, chills, confusion
Pharmily offers free blood pressure monitoring at our Muthaiga location and can teach you home monitoring techniques during a teleconsultation.
Nutrition Support
Cook in batches when the patient has a "good day"; freeze portions
Use insulated flasks to keep uji warm for frequent small meals
Blend traditional foods into smoothies if chewing is difficult
Keep oral rehydration salts handy (diarrhea is common)
Gentle bathing: Use warm water, mild soap (like Dettol or Lifebuoy gentle care)
For bedridden patients: Change position every 2 hours to prevent sores
Keep skin moisturized—cancer drugs dry the skin dramatically
Pharmily stocks: Gentle cleansers, pressure relief cushions, and skin barrier creams
Doctors are rushed. Come prepared:
Start with the most critical issue first
Use your symptom tracker: "Last Tuesday, pain was 7/10"
Ask: "If this happens again, when should I call you?"
Request written instructions—verbal advice is forgotten
Cancer affects the whole family. Hold brief weekly meetings to:
Update everyone on the patient's status
Delegate tasks: "John handles pharmacy runs, Mary handles meals"
Share the financial burden transparently
Give children age-appropriate roles—they need to help, not feel helpless
Some days they'll want to talk; other days they'll retreat. Follow their lead. Avoid toxic positivity ("Just stay strong!") and acknowledge reality: "This is really hard. I'm here."
You are the engine of this operation. If you break down, everything stops.
5 minutes alone: Step outside, breathe deeply
One meal eaten sitting down: Not standing at the kitchen counter
Sleep in 4-hour blocks: If nighttime care disrupts sleep, nap when the patient naps
One task delegated: "Please buy sukuma wiki today"—practice asking for help
Ask one person for concrete help: "Can you sit with mum Saturday 2-4 PM while I rest?"
Do one thing that feels like "you": Listen to music, call a friend, attend church
Check your own health: Take your blood pressure, notice if you're getting sick
Attend one caregiver support meeting (even virtual)
Review finances: Where can you cut costs? Pharmily's monthly refill discount saves 10-15%
Evaluate the care plan: What's working? What needs to change?
You cannot do this alone. Actively build your team:
Medical: Oncologist, pharmacist, home nurse (if affordable), telemedicine doctor
Emotional: Support group, trusted friend, counselor, pastor
Practical: Family members, neighbors, church members, NGOs
Financial: SHIF, MP, welfare groups, Pharmily's affordable medication plans
Kenya Cancer Association - support groups and financial advice
Faraja Cancer Trust - counseling and emergency funds
Pharmily Care - home delivery of medications, teleconsultations, caregiver support
Hospices of Kenya - palliative care guidance
Need caregiver support, medication delivery, or professional guidance?
Pharmily is your care partner:
Phone: +254726669898 (24/7 pharmacist support)
Location: Muthaiga Business Center, Nairobi
License No. P2024d02679
Free delivery in Nairobi for orders above Ksh 2,999
Caregiver discount: 10% off monthly with patient treatment card
You care for them. We care for you.
1. How do I manage giving multiple medications at different times without making mistakes?
Use a weekly pill organizer with 4 compartments per day (morning, afternoon, evening, bedtime). Set labeled phone alarms. Write the schedule on paper and tape it to the fridge. Pharmily pharmacists can create a simplified medication chart during a free consultation.
2. What should I do if the patient refuses to take their medication?
First, understand why: Is it nausea? Fear? Confusion? Address the root cause. For nausea, ask about anti-nausea medication. For fear, involve the doctor in explaining benefits. For confusion, simplify the routine. Never force—seek professional guidance.
3. How can I afford caregiving if I have to quit my job?
Explore all income sources: SHIF Chronic Disease Support, MP's CDF funds, family contributions, and NGO grants. Consider part-time telecommuting. Use services like Pharmily's free delivery to save transport costs and time. Some caregivers earn income through small home businesses during patient rest times.
4. How do I tell when I'm burning out versus just having a hard day?
Burnout is persistent: feeling detached, hopeless, or resentful for weeks; getting sick frequently; or having thoughts of walking away. Hard days come and go. If you experience burnout signs, seek help immediately from a counselor or support group. Pharmily offers tele-counseling for caregivers.
5. What are the most important things to track and tell the doctor at each appointment?
Track: Daily pain levels (0-10 scale), appetite changes, new symptoms, medication side effects, sleep quality, and mood changes. Bring: Your medication list, symptom log, questions list, and financial concerns. The more specific you are ("Tuesday night fever of 38.5°C lasted 3 hours"), the better the doctor can help.