Date: 17 Dec 2025
Diarrhea is more than just loose stools — it’s a signal that something in your digestive system is off. In this detailed article, we unpack what diarrhea is, the different types, causes, symptoms, risks, and how to treat and prevent it.
We also explore how to manage dehydration, a major complication, and provide practical tips rooted in global health guidance.
Whether you're a caregiver, a traveler, or someone just wanting to understand better, this guide gives you actionable information.
What Is Diarrhea?
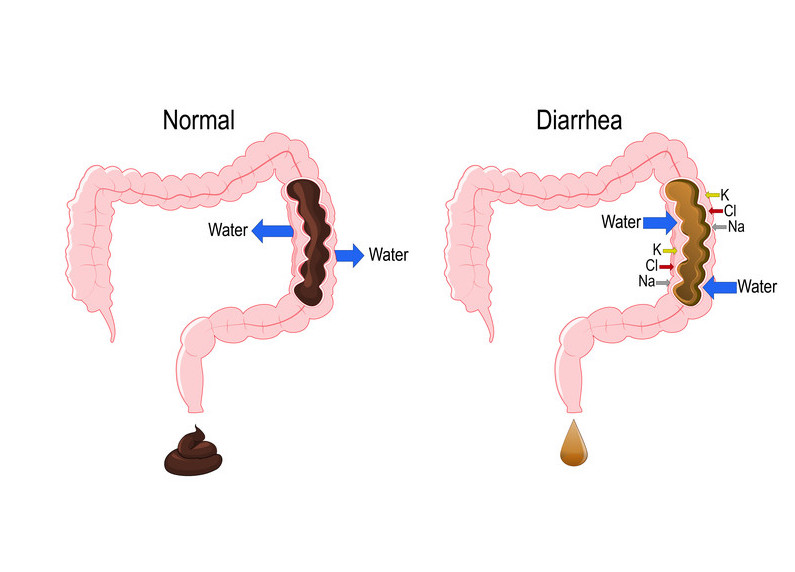
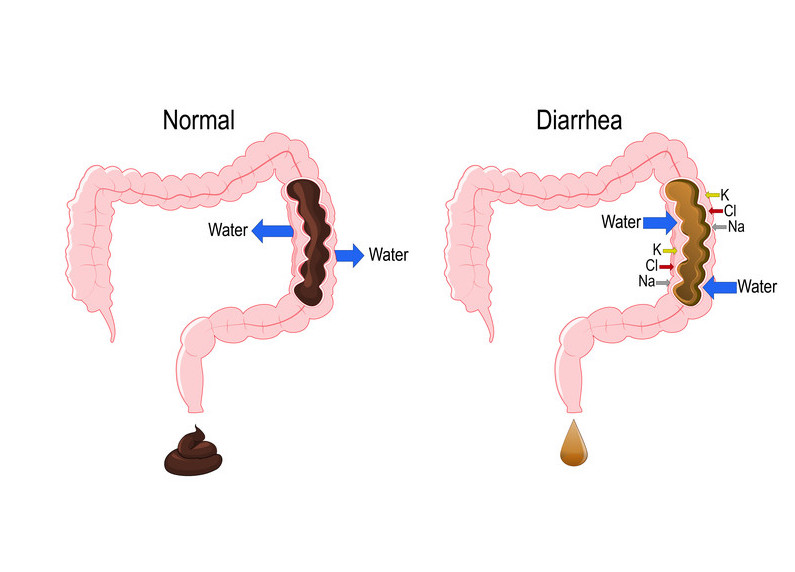
Diarrhea is the condition of passing three or more loose or watery stools in a day, or more frequently than is normal for the individual.
It typically indicates increased fluid secretion or reduced absorption in the intestines, leading to more water in stool.
Although often temporary, diarrhea can become dangerous, especially when it leads to dehydration.
Types of Diarrhea
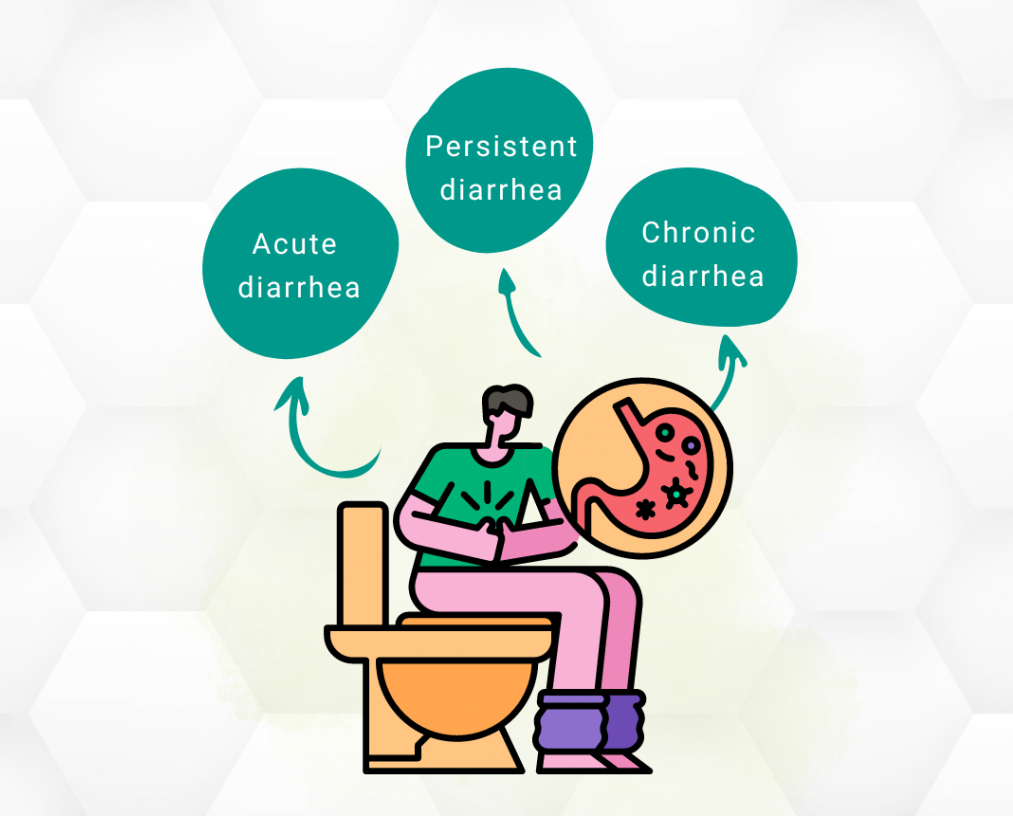
Understanding the type of diarrhea helps with treatment. According to the World Health Organization (WHO), there are three main clinical types:
- Acute Watery Diarrhea
This is the most common form, lasting from a few hours to several days. It often includes infections like cholera.
- Acute Bloody Diarrhea (Dysentery)
Here, you may notice blood in the stool. This type often points to bacterial infection (e.g., Shigella) and requires prompt medical evaluation.
- Persistent Diarrhea
Persistent diarrhea lasts 14 days or longer. It is more common in children in resource-limited settings and can contribute to malnutrition.
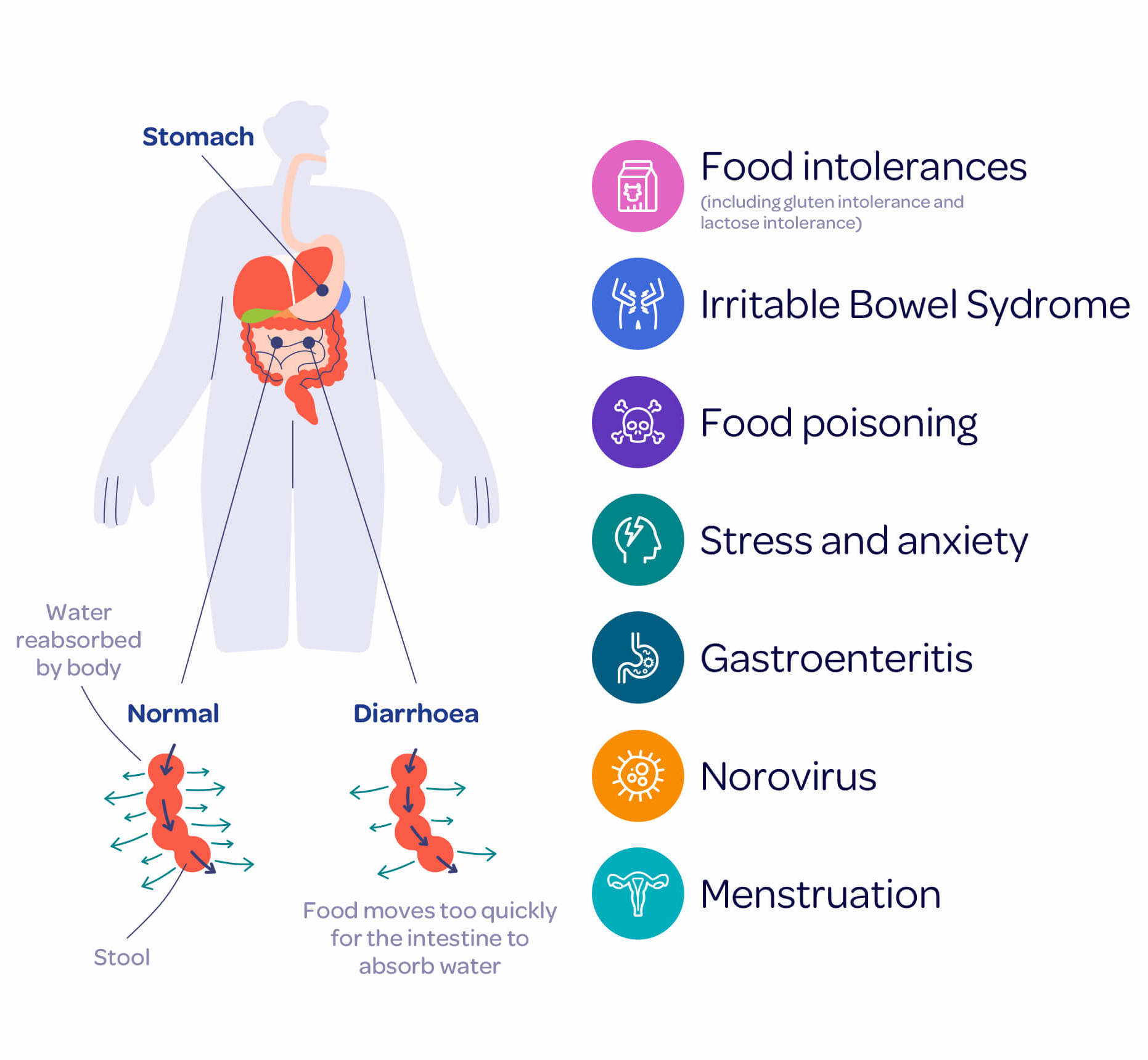
Causes of Diarrhea
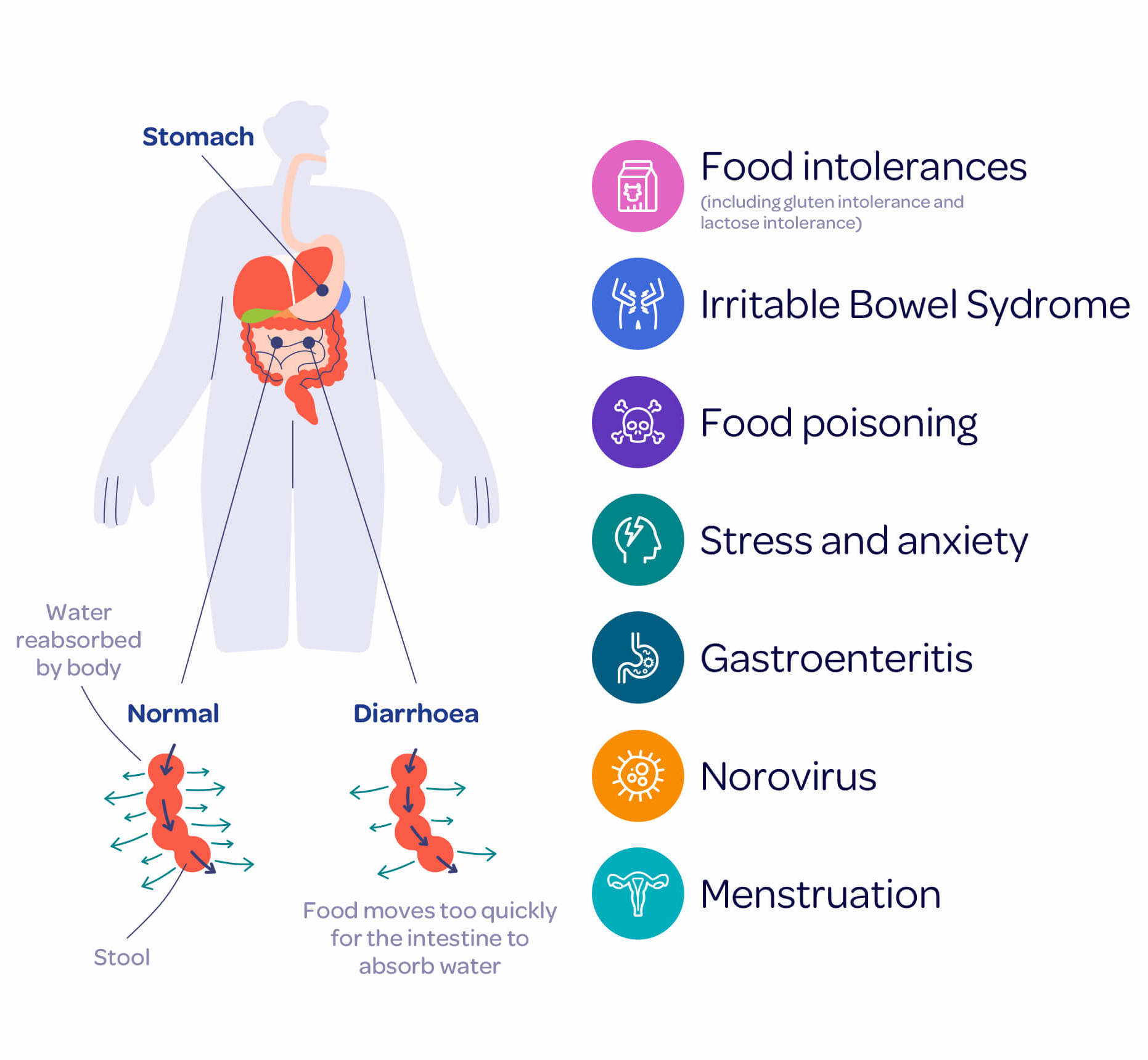
A variety of factors can trigger diarrhea. Some of the most common causes include:
- Infectious agents: Bacteria (such as E. coli or Salmonella), viruses (like rotavirus or norovirus), and parasites can infect the gastrointestinal tract.
- Contaminated food or water: Many diarrheal diseases spread through the fecal–oral route, especially in areas with poor sanitation.
- Poor hygiene: Not washing hands properly, especially after using the toilet or before handling food, increases risk.
- Other factors: Chronic conditions, medications, or malabsorption syndromes can also lead to diarrhea.
Signs and Symptoms
When you have diarrhea, you may experience several symptoms, often simultaneously:
- Frequent loose stools: Passing watery or loose stool three or more times a day is a hallmark.
- Abdominal cramping or pain: Many people report stomach cramps, urgency, or bloating.
- Nausea or vomiting: Depending on the cause, you might feel nauseous or throw up.
- Weight loss: Chronic diarrhea may lead to weight loss, especially if it affects nutrient absorption.
- Dehydration symptoms: These include extreme thirst, dry mouth, dark urine, dizziness, or lethargy.
The Biggest Risk: Dehydration
One of the most serious complications of diarrhea is dehydration. When diarrheal fluid losses are not replaced, the body loses water and vital electrolytes.
Dehydration from diarrhea manifests with signs such as excessive thirst, reduced urination, dry skin, sunken eyes, and fatigue.
In severe cases, dehydration can lead to low blood pressure, shock, or even death if not managed appropriately.
Diagnosis
When someone has persistent or severe diarrhea, a health professional may need to determine the cause and assess for complications. Diagnostic steps often include:
- Medical history: Questions about onset, duration, stool frequency, and any blood.
- Stool tests: Examining stool for bacteria, parasites, or blood may help identify the cause.
- Physical exam and labs: A clinician may check for signs of dehydration and perform blood or urine tests to assess electrolyte balance.
Treatment and Management
Treating diarrhea focuses on two main goals: rewater + replace electrolytes, and address the underlying cause.
- Rehydration
- Use oral rehydration solution (ORS): A mix of sugar, salt, and clean water recommended by WHO saves lives.
- For mild diarrhea, sipping water, broths, or juices can help restore fluid balance.
- In severe or persistent dehydration, intravenous (IV) fluids may be required under medical supervision.
- Medication and Other Therapies
- Antimicrobials may be prescribed if a bacterial cause is suspected, especially in cases with blood or high fever.
- In children, zinc supplementation has been shown to reduce the duration and severity of diarrheal episodes.
- Diet should resume as soon as rehydration begins. For infants, breastfeeding should continue without unnecessary interruption.
Prevention Strategies
You can significantly lower the risk of diarrhea by adopting preventive measures. Some key strategies include:
- Good hygiene: Wash your hands frequently with soap, especially before eating or after using the toilet.
- Safe water and sanitation: Use treated or boiled water for drinking. Ensure good sanitation infrastructure to limit contamination.
- Vaccination: Vaccines against rotavirus, a common cause of severe diarrhea in children, are recommended.
- Proper nutrition: Exclusive breastfeeding for the first six months protects infants from diarrheal diseases.
- Travel precautions: When traveling, especially to areas with poor sanitation, choose bottled or boiled water and avoid raw foods.
When to Seek Medical Help
While many cases of diarrhea improve with simple home care, sometimes medical attention is necessary. Consult a healthcare provider if:
- The diarrhea lasts more than 48 hours in an adult, or 24 hours in a child.
- There is blood or pus in the stool, which may signal infection.
- You notice signs of severe dehydration: inability to drink, very little or no urination, sunken eyes, or lethargy.
- You have very high fever, or you are already medically vulnerable (older age, weakened immune system).
Complications of Untreated Diarrhea
If diarrhea is left unattended, particularly with dehydration, you may face serious problems:
- Hypovolemic shock: Extreme fluid loss can lead to dangerously low blood volume and shock.
- Kidney issues: Persistent dehydration stresses the kidneys and may result in kidney failure or stones.
- Electrolyte imbalance: Losing salts like sodium and potassium can disrupt nerve and muscle function.
- Malnutrition: In children especially, recurrent diarrhea can impair nutrient absorption and stunt growth.
Diarrhea in Special Populations
- Infants and young children: They dehydrate faster and may not be able to express thirst. Caregivers should watch for fewer wet diapers, sunken fontanelles, or no tears when crying.
- Older adults: They may have a reduced sense of thirst, making dehydration less obvious.
- Travelers: Regions with poor water quality pose a high risk; precautions like bottled water and ORS are vital.
- People with chronic illness: Conditions such as inflammatory bowel disease or medications may make them more vulnerable.
Practical Tips at Home
- Start rehydration immediately — As soon as diarrhea begins, begin sipping ORS or electrolyte-rich fluids.
- Eat wisely — Choose bland, easy-to-digest foods (such as rice, toast) when appetite returns.
- Keep clean — Wash utensils and hands regularly to avoid spreading infection.
- Avoid irritants — Temporarily limit caffeine, alcohol, and very fatty foods until recovery.
- Monitor — Record fluid intake, stool frequency, and any concerning symptoms; this helps if you need to consult a doctor.
Diarrhea is a common but potentially serious condition. While it often resolves on its own, the greatest risk — dehydration — requires prompt and effective action.
By prioritizing rehydration, maintaining hygiene, and knowing when to seek medical help, you can manage most episodes safely.
Public health measures such as clean water access, sanitation, and vaccination also play a crucial role in reducing the global burden of diarrheal disease.
For trusted and authoritative information, you can refer to global health resources like the World Health Organization.
FAQs
Q1: How long does diarrhea usually last?
A: Acute diarrhea often resolves in a few days, especially with rehydration. But if it persists beyond two days (or 24 hours in children), you should seek medical advice.
Q2: Can antibiotics treat all diarrhea?
A: No. Antibiotics are only effective when diarrhea is caused by certain bacteria. Viral or parasitic diarrhea will not respond to antibiotics; overuse can be harmful.
Q3: Is homemade oral rehydration solution effective?
A: Yes. The WHO-recommended formula — clean water, salt, and sugar — works well for most cases and is cost‑effective.
Q4: Can I prevent diarrhea when traveling?
A: To a large extent, yes. Use safe drinking water, avoid raw or uncooked foods, and practice strict hand hygiene.
Q5: When is diarrhea life-threatening?
A: Diarrhea becomes dangerous when dehydration sets in, especially in children, the elderly, or people with weak immune systems. Also, bloody diarrhea or very high fever signals a need for urgent care.