Date: 03 Oct 2025
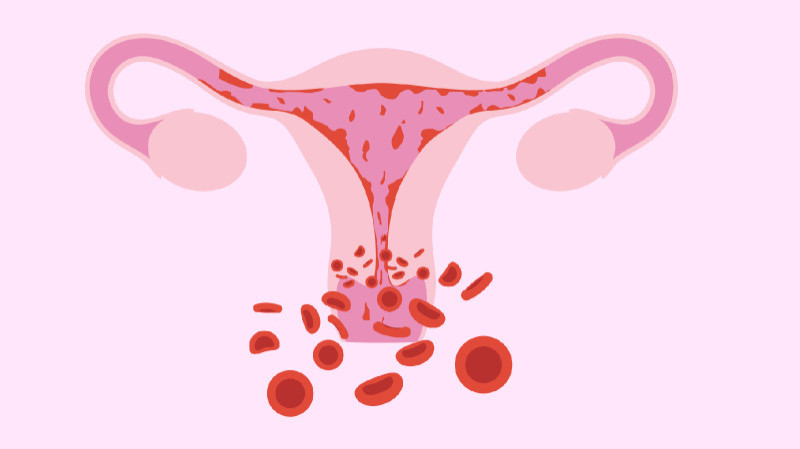
Menorrhagia refers to menstrual bleeding that is abnormally heavy or prolonged—typically lasting more than 7 days, or involving passage of large blood clots or frequent changes of sanitary products (e.g. soaking through a pad every hour). This can lead to iron‑deficiency anemia, fatigue, reduced quality of life, and emotional distress.
Common contributors to menorrhagia include:
Heavy menstrual bleeding, or menorrhagia, often has multiple causes. It usually results from one or more of the following conditions:
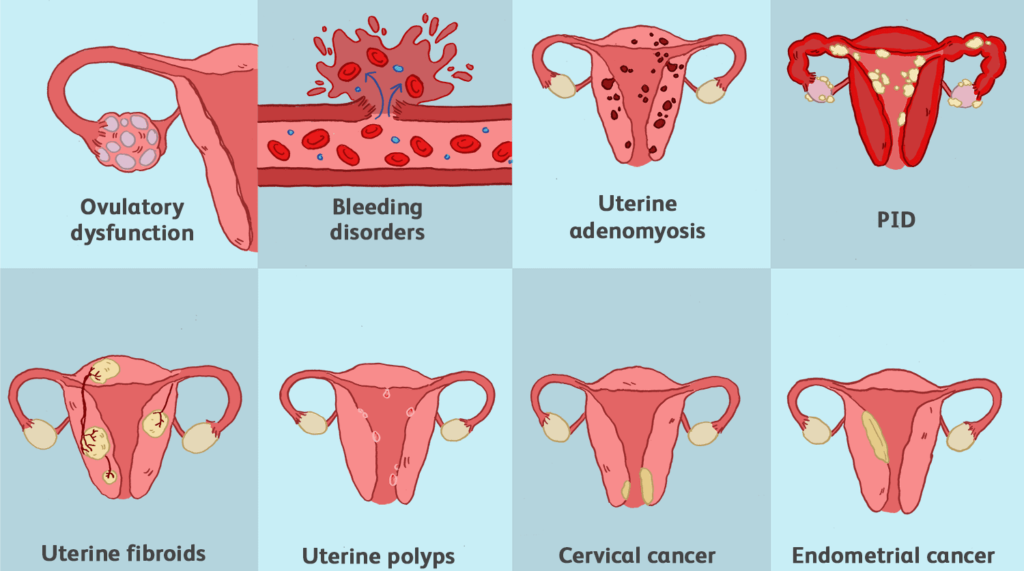
Benign growths like fibroids, polyps, and adenomyosis, or conditions like endometrial hyperplasia, can increase bleeding by enlarging the uterine lining or distorting the uterus. These changes disrupt normal shedding and contraction, making periods heavier.
When ovulation doesn't occur (anovulation), estrogen builds up the uterine lining without progesterone to balance it. This leads to excessive growth and heavy shedding. Common in PCOS, thyroid issues, obesity, and perimenopause.
Conditions like von Willebrand disease or platelet function defects impair clotting, causing prolonged bleeding. Many women discover these disorders only after experiencing menorrhagia.
Chronic infections like PID or endometritis, often caused by STIs such as chlamydia or gonorrhea, can inflame the uterus and increase bleeding by damaging the lining.
Heavy bleeding may signal complications like miscarriage, ectopic pregnancy, retained tissue, or molar pregnancy. These are not menstrual but require urgent care.
Diseases like liver/kidney problems or blood cancers can affect clotting. Blood thinners and some IUDs may also worsen bleeding.
Key Insight: In many women, multiple factors contribute simultaneously (e.g. fibroid + hormonal imbalance + mild bleeding disorder). That’s why an individualized diagnostic approach is essential.
A comprehensive evaluation helps tailor treatment:
Treatment should aim to:
When fibroids or large polyps are identified, surgical removal—via hysteroscopy, myomectomy, or endometrial ablation—can drastically reduce bleeding. These interventions restore uterine integrity and often provide long-term relief for women experiencing structural causes of heavy periods.
If PID is diagnosed, a treatment course involving broad-spectrum antibiotics is prescribed. Prompt therapy not only resolves infection, but also helps stabilize menstrual cycles and reduce excessive bleeding caused by inflammation.
Hormonal dysfunction is frequently corrected using combined oral contraceptives (COCs) or high-dose progestin therapy. These medications regulate the endometrial lining, slow its buildup, and stabilize bleeding. In some cases, intrauterine devices (IUDs) releasing levonorgestrel are used for continuous bleeding control.
NSAIDs are commonly used to manage ovulatory menorrhagia. They work by reducing prostaglandin levels in the uterine lining—chemicals that contribute to both bleeding and cramping. By lowering these levels, NSAIDs help decrease menstrual blood loss and relieve pain. Clinical studies show that NSAIDs can reduce menstrual bleeding by 20% to 46%.

These pharmacy products offer supportive care during treatment of heavy bleeding:
A highly absorbable, stomach-friendly iron supplement ideal for managing anemia due to menorrhagia. Its liposomal delivery ensures higher uptake with minimal gastrointestinal side effects.
Iron bisglycinate is known for its superior absorbability and tolerability. Formulated with Vitamin C, B12, and folic acid, this supplement helps rebuild healthy blood levels and combat fatigue. Why it stands out: Specifically designed for iron deficiency and especially helpful for women with heavy menstrual bleeding.
This liquid iron formula is flavored and easy to take, ideal for those who dislike pills. Enriched with B vitamins and minerals, it supports red blood cell production and energy. Why it stands out: Delicious flavor, gentle on the stomach, and ideal for ongoing supplementation during treatment.
Here’s how you can combine medical treatment with supportive supplements:
Consult your healthcare provider if: