Date: 17 Dec 2025
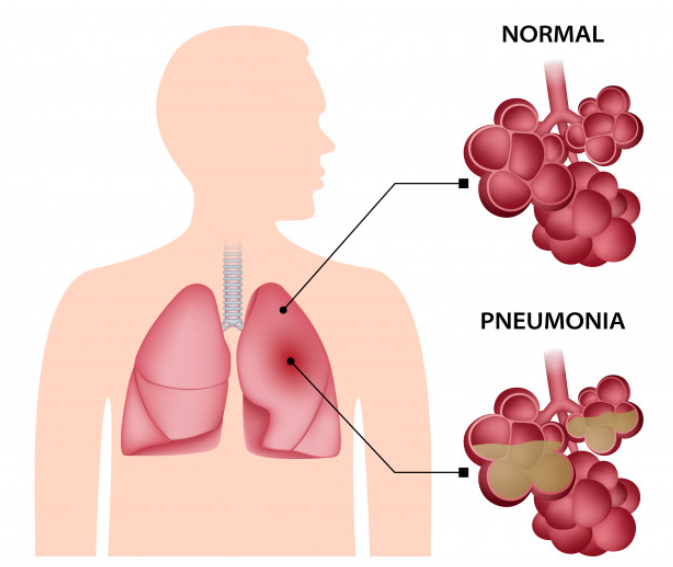
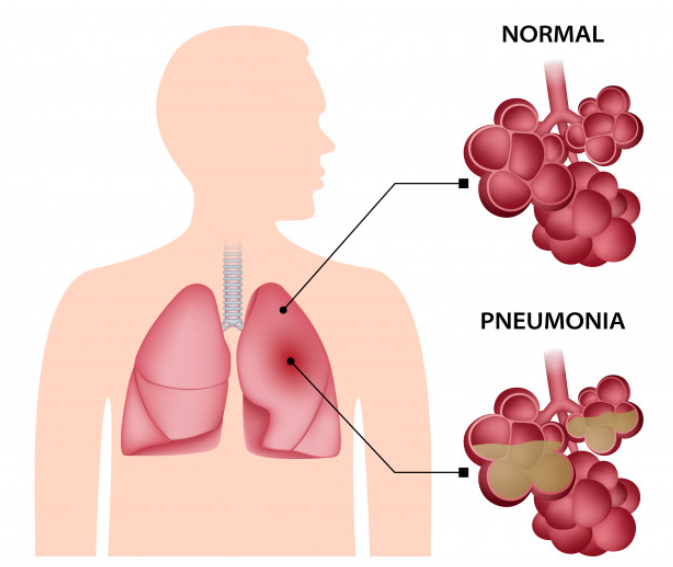
Pneumonia is a serious infection of the lungs marked by inflammation of the tiny air sacs (alveoli), which can fill with fluid or pus. This buildup makes breathing painful and reduces oxygen transfer into the bloodstream.
The disease can range from mild to life-threatening, depending on the person’s age, immune status, and the infecting organism.
Why Pneumonia Matters: The Global Impact
Pneumonia remains one of the most significant infectious diseases worldwide. According to the World Health Organization (WHO), it is the leading infectious cause of death in children under 5.
Risk is especially high for young children, older adults (65+), and people with weakened immune systems. Moreover, in severe cases, pneumonia can lead to complications such as bacteremia (bacteria in the blood) or lung abscesses.
Types of Pneumonia
Pneumonia is not a single disease but has different forms, depending on how it’s acquired and what causes it:
- Community-acquired pneumonia (CAP): This is the most common type and occurs outside hospitals.
- Hospital-acquired pneumonia: Develops during a hospital stay, especially in patients on ventilators.
- Health care–acquired pneumonia: Occurs in people who receive outpatient care or live in long-term care facilities.
- Aspiration pneumonia: Happens when someone inhales food, drink, or saliva into their lungs, often due to impaired swallowing reflexes.
- Viral, Bacterial, and Fungal pneumonia: Based on the pathogen, pneumonia can be caused by viruses, bacteria, or fungi.
What Causes Pneumonia?
Pneumonia’s root causes are varied, and understanding them helps in prevention and treatment:
- Bacterial infections: One of the most common causes is Streptococcus pneumoniae. Others include Mycoplasma pneumoniae and Haemophilus influenzae.
- Viral infections: Viruses like influenza, COVID-19, and respiratory syncytial virus (RSV) can lead to pneumonia.
- Fungal infections: Less common, these occur especially in people with weakened immune systems.
- Aspiration: Inhaling foreign particles (food, drink, vomit) can bring pathogens into the lungs.
Who Is at Risk? (Risk Factors)
Certain people face a higher risk of developing pneumonia. These include:
- Young children (especially under 2 years): Their immune systems are still developing.
- Older adults (65+): Age weakens natural lung defenses.
- People with chronic illnesses: Conditions like COPD, heart disease, or diabetes raise the risk.
- Weakened immune systems: Immunosuppressive therapies, HIV, or organ transplants can predispose someone.
- Smokers: Smoking damages lung defenses, making infection more likely.
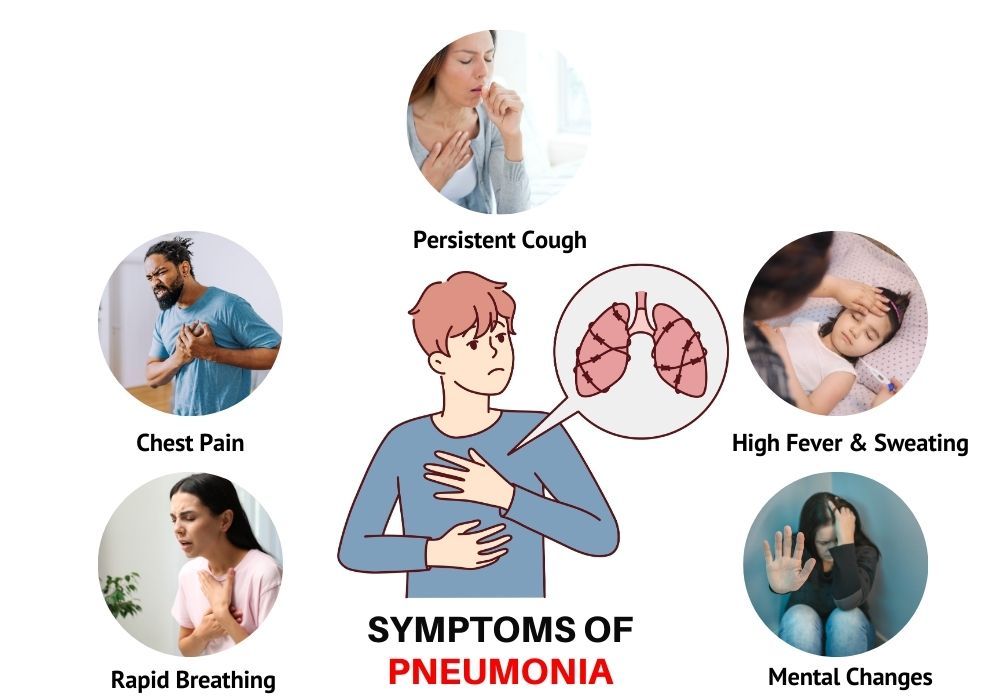
Common Symptoms of Pneumonia
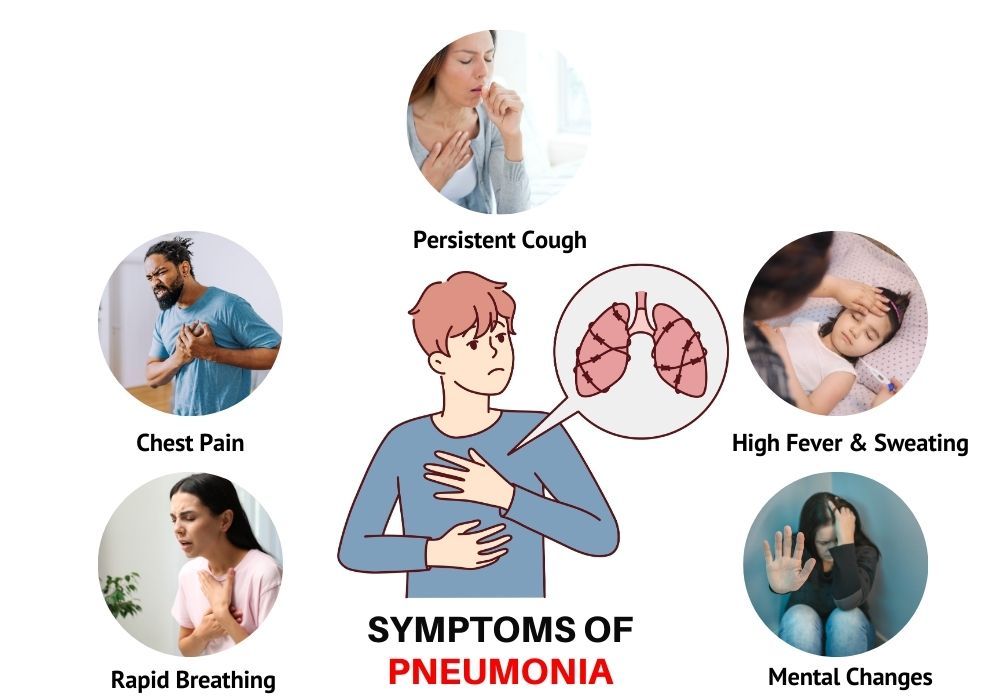
Symptoms of pneumonia vary, but common signs include:
- Persistent cough: Often produces phlegm or mucus.
- Fever, chills, and sweating: These systemic signs show the body is fighting infection.
- Shortness of breath: Breathing becomes difficult due to fluid in the lungs.
- Chest pain: Pain can worsen when breathing deeply or coughing.
- Fatigue: The infection drains energy, leaving sufferers very tired.
- Confusion (especially in older adults): This may be a sign of low oxygen or systemic infection.
- Gastrointestinal symptoms: Nausea, vomiting, or diarrhea can also accompany pneumonia.
How Is Pneumonia Diagnosed?
Doctors use several methods to diagnose pneumonia, often combining them for accuracy:
- Physical exam: Listening to the lungs with a stethoscope often reveals crackling or bubbling sounds.
- Chest X-ray: Imaging helps confirm the presence of fluid or consolidation in the lungs.
- Blood tests: These can detect elevated white blood cell counts or markers of infection.
- Sputum culture or swab: A sample from the cough can identify the specific pathogen.
- Pulse oximetry: Measures blood oxygen levels to see how well lungs are functioning. (Though this is standard practice, the sources above imply respiratory assessment.)
Treatment and Management of Pneumonia
Treatment depends on the type and severity of pneumonia, but key strategies include:
- Antibiotics: These are used when bacteria cause pneumonia.
- Antiviral drugs: In viral pneumonia (like influenza or COVID-19), antivirals may help if available and indicated.
- Antifungal medications: For fungal pneumonia, antifungal therapy may last several weeks or months.
- Supportive care: Rest, hydration, oxygen therapy (if needed), and fever reducers like acetaminophen or ibuprofen are very important.
- Hospitalization: Severe cases, or those in high-risk groups, may require hospital care, oxygen support, or even ventilatory support.
Potential Complications
Pneumonia, if not treated or if very severe, can lead to serious complications:
- Bacteremia (sepsis): The infection may enter the bloodstream and spread to other organs.
- Pleural effusion: Fluid can build up around the lungs, sometimes requiring drainage.
- Lung abscess: Pus may form inside the lung in a pocket called an abscess, possibly needing surgery or drainage.
- Respiratory failure: In severe pneumonia, breathing may become dangerously inadequate, necessitating intensive care.
Preventing Pneumonia: What You Can Do
Prevention is always better than cure. Here are proven ways to reduce your risk:
- Vaccination: Getting vaccinated is one of the most effective ways to prevent pneumonia. Vaccines include pneumococcal vaccines, influenza (flu) shots, and others.
- Good hygiene: Regular handwashing and using alcohol-based sanitizers lower the risk of respiratory infections.
- Quit smoking: Smoking damages lung defenses, so stopping greatly reduces risk.
- Healthy lifestyle: Eating a balanced diet, exercising regularly, getting enough sleep — all strengthen your immune system.
- Reduce indoor pollution: Poor air quality, such as from indoor smoke (e.g. from cooking), increases pneumonia risk.
Living with Pneumonia: Recovery and Aftercare
Recovering from pneumonia takes time and care. Even after symptoms ease, your lungs might still need support:
- Stay hydrated: Drink plenty of fluids to thin mucus and help your body clear the infection.
- Rest adequately: Avoid strenuous activities until fully recovered, because your body needs energy to heal.
- Use a humidifier: Moist air helps loosen mucus and eases breathing.
- Follow medical advice: Take all prescribed medication, even if you feel better early.
- Monitor oxygen levels: If you've had severe pneumonia, checking with a pulse oximeter at home (if advised) may help you ensure your blood oxygenation is stable.
Pneumonia is a serious but manageable lung infection. Understanding its causes, symptoms, and risk factors empowers you to take preventive action. With timely diagnosis and appropriate treatment, most people recover well.
By promoting vaccination, good hygiene, and a healthy lifestyle, we can reduce the global burden of pneumonia – especially among the most vulnerable.
FAQs
Q1: Is pneumonia contagious?
Yes, pneumonia can be contagious depending on its cause. Viral and bacterial forms may spread when an infected person coughs or sneezes. Good hygiene and vaccination help reduce transmission.
Q2: How long does pneumonia last?
The duration varies. Mild pneumonia often improves within a week or two with treatment, but full recovery may take several weeks.
Q3: Can pneumonia be prevented by a vaccine?
Absolutely. Vaccines against pneumococcal bacteria and influenza (flu) reduce the risk of pneumonia significantly.
Q4: When should I see a doctor for pneumonia?
You should seek medical care if you experience difficulty breathing, chest pain, persistent or high fever, confusion (especially in the elderly), or a cough that lasts many days.
Q5: Can pneumonia recur?
Yes, especially in people with risk factors like weakened immunity, chronic lung disease, or those who smoke. Preventive measures and vaccinations help reduce recurrence.